Regulatory Considerations
What is needed to become a telemedicine provider?
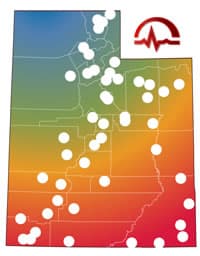
State Licensure
Utah Division of Occupational and Professional Licensing (DOPL) requires providers be licensed in Utah to provide care to our residents. The Division of Occupational and Professional Licensing, also known as DOPL, is one of seven agencies within the Utah Department of Commerce. DOPL is legislatively charged to administer and enforce specific laws related to the licensing and regulation of certain occupations and professions.
The provider is under the jurisdiction of the licensure laws in the state where the patient is located. The State Medical Board or specific Professional Licensure Boards, Colleges or Associations administer laws and requirements to determine professional standards and practice.
With the burgeoning use of telecommunication and other technologies, practice is no longer limited by geographical boundaries. Many professional organizations are exploring Cross State Licensure Agreements or Compacts to streamline the licensure process while maintaining patient safety. Reciprocity is dependent on a state demonstrating that their requirements for licensure meet the standards required by other participating jurisdictions.
- The State Federation of Medical Boards is working towards an Interstate Medical Licensure Compact.
- The Interstate Nurse Licensure Compact (NLC), a mutual recognition licensure model for nurses, has 24 member states. The NLC allows nurses to have one multistate license, with the ability to practice in both their home state and other compact states.
- The Association of State and Provincial Psychology Boards encourages states and provinces to enter into a cooperative agreement whereby any individual holding a license in one AOR participating jurisdiction may obtain a license to practice in another AOR participating jurisdiction.
Specialty Practice Standards
Generally, to practice safe telemedicine, the standard of care applied by a practitioner must be the same standard required of the practitioner for an in-person visit. Many guidelines recommend that telemedicine provide the practitioner with information equal to or superior to an in person examination and that a physician-patient relationship is established. In 2014, the American Medical Association (AMA) adopted a Coverage of and Payment for Telemedicine H-480.946.
Some common themes in the practice standard guidelines are:
- Establishing the patient-physician relationship
- Verifying patient identity and location
- Disclosing provider credentials and identity
- Obtaining informed patient consent
- Prescribing is held to the same standard as other treatments
- Provide continuity of care on how to access follow up care or information from the provider
- A referral process for emergency services
- Records must be complete and accessible
There have been attempts in some states to impose different and more stringent medical practice standards for telemedicine compared to in-person care. This includes requirements for an pre-established relationship in-person, in-person examination before a telemedicine encounter, telepresenter or facilitator, in-person follow-up visits, limitations on allowable telemedicine technology, prescribing and patient settings.
- Malpractice Liability and Insurance
- Providers performing telemedicine services should ensure that their malpractice liability insurance policy covers telemedicine in all of the States they are practicing telemedicine.
- Questions to ask your telemedicine malpractice carrier:
- Does my liability insurance cover telemedicine services?
- Do you cover all states that I am licensed in and provide telemedicine services?
- Are there any technology standards or protocols that you recommend I follow?
- Am I covered if there is a failure to use telemedicine when its use is alleged to be required under the applicable standard of care?
- Are my policy limits adequate in each state? For example, if I practice in a state with a cap on damages, am I insured to the level of that cap?
- What is your rating, by AM Best or by any comparable rating organization?
- What has been your claims experience with distance care in my specialty in each state where I practice or plan to practice?
- Do you offer a consent-to-settle clause? If so, is it offset by a "hammer" clause?
- Do you offer any telemedicine-specific risk management advice?
- Do you offer any premium discount if I take relevant CME or similar courses designed to reduce my risk, and therefore yours?
- Some common causes of liability claims for face to face encounters are:
- errors in diagnosis
- medication errors
- failure to monitor the patient
- treatments that were not indicated
- Some liability considerations are:
- Are you following the standards of conventional care?
- Are you following the practice standards set by the State the patient is located?
- Have you established a patient-physician relationship? The definition of the patient-physician relationship varies from State to State. Generally, a relationship has been established when individual advice is given to the patient.
- Do you have access to the patient’s medical records and past history? The patient doesn’t always know their medical history.
- Have you documented the patient encounter, including the patient’s understanding & instruction method? How will this documentation be shared with the patient and the patient’s primary care provider?
- What are the prescriptions standards in the State where the patient is located?
- What is your patient follow-up plan and how will you get them back into the system?
- Do you have a method for reporting any discrepancies?
- Are you licensed in the State and appropriately credentialed at the patient location?
- Are you adhering to the HIPAA patient privacy standards?
- Are use using quality technology solutions and secure networks?
- What are your technology standards and protocols?
- Do you have a backup communication plan, in the event you have technical problems or an emergency plan, if the patient needs assistance?
- Failure to using telemedicine when it is available may be an issue
- AMA - advises physicians to make sure their liability insurance covers telemedicine services.
- Telehealth Resource Center Medical Malpractice and Liability
- ATA Telemedicine Practice Guidelines
“ATA’s practice guidelines for telemedicine are the critical foundation for the deployment of telemedicine services. Practice guidelines form the basis for uniform, quality patient care and safety, grounded in empirical research and clinical experience.”- HHS HIPAA and Telehealth
- Documentation – it is best to document information about the patient location and other information required by third party payers to meet reimbursement eligibility and to comply with the recommend professional standards. Documentation should meet the standard for your healthcare facility and include information on the patient encounter, including the patient’s understanding & instruction method. Documentation needs to be accessible to the patient and their primary care provider to ensure continuity of care.
The resources presented on this website, and on the webpages accessible through the links on this page, are provided for informational purposes only. This information is not intended to be comprehensive and the manner in which it applies to your organization will be unique. You should seek expert advice to ensure that you are taking into account all relevant considerations. The UETN does not provide legal advice. If the resources that you find here do not answer your questions to your satisfaction, you should consult a lawyer or other qualified expert.